Am I a Good Candidate for Dental Implants?
Short answer: Yes — most adults are good candidates for dental implants.
Only a small number of patients need gum therapy, bone augmentation, or medical stabilisation before the implant can be placed.
At Maple Dental Health, implant assessments are carried out by Dr. Carly Gordon, Dr. Lulu Shen, Dr. Jane Wu, Dr. Mirette Mounir, and Dr. Nitish Manna, who evaluate gum stability, bone quality, medical history, bite forces, and healing-related factors before recommending treatment.
Why patients choose implants
Dental implants behave much like natural teeth once healed. They stay firmly anchored during chewing, preserve bone structure, and do not shift the way removable dentures can.
Patients typically choose implants for:
- long-term predictability
- comfort and stability
- preservation of jawbone
- ability to support crowns, bridges, or full-arch restorations
As Dr. Carly Gordon explains, “Patients appreciate that implants offer a fixed, durable solution. They want something that feels natural and will last.”
What candidacy involves
Patients often ask whether they are “allowed” to have an implant. Implant candidacy is rarely an absolute yes or no — it is about establishing a healthy foundation.
Dentists assess:
- gum health
- bone height and width
- systemic health
- medications
- bite dynamics
- hygiene habits
- reason for tooth loss
If something needs improvement, the implant is delayed until the environment is stable.
“We aim for predictable healing, not rushed timelines,” notes Dr. Lulu Shen.
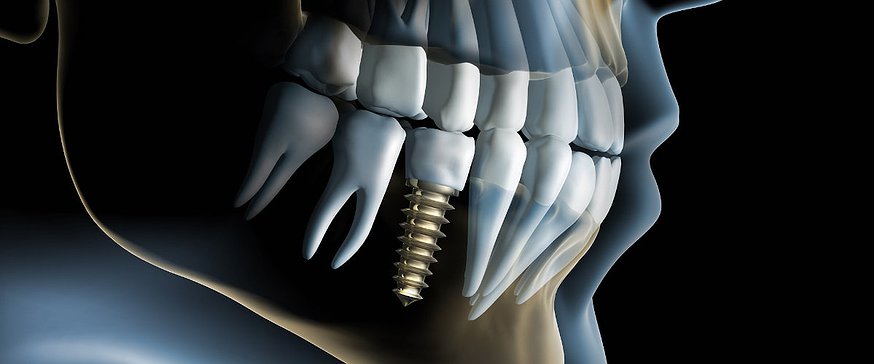
Bone requirements
Strong, healthy bone is essential.
Two measurements matter:
- Bone height — space above the nerve or sinus
- Bone width — enough thickness to hold the implant securely
Common patterns of bone loss seen in practice:
- Upper back teeth: sinus expansion after extraction
- Lower molars: gradual narrowing of the ridge
- Lower front teeth: naturally thin bone
- Areas previously affected by periodontal disease: deeper structural loss
If bone is insufficient, dentists may recommend:
- socket preservation after extraction
- ridge augmentation
- sinus lift
- minor particulate grafting at the time of implant placement
Bone loss rarely disqualifies a patient permanently; it simply adds a preparatory step.
Gum and periodontal stability
Healthy gums support long-term implant success.
Dentists evaluate:
- bleeding on probing
- pocket depth
- calculus under the gums
- mobility of neighbouring teeth
- presence of gum recession
If active periodontal disease is present, treatment is completed first. This might involve deep cleaning, antimicrobial therapies, or structured maintenance appointments.
According to Dr. Jane Wu, “A history of gum disease does not prevent someone from receiving an implant. What matters is current stability and consistent maintenance.”
General health and medications
Age does not restrict candidacy. Many excellent implant cases involve patients in their 60s and 70s.
Conditions that require careful management:
- poorly controlled diabetes
- immune suppression
- recent chemotherapy
- long-term high-dose steroid use
- bleeding disorders
- heart conditions requiring medical clearance
Controlled diabetes is usually acceptable; uncontrolled diabetes increases healing risk.
Medications affecting bone turnover — such as intravenous bisphosphonates — require coordination with the patient’s physician.
Lifestyle and habits
Daily habits influence healing:
Smoking
Nicotine reduces blood supply to healing tissues. Smokers have a higher complication rate. Some are advised to reduce smoking during recovery.
Bruxism (night grinding)
Grinding can overload implants. A night guard often protects the restoration.
Oral hygiene
Regular home care helps prevent inflammation around the implant.
Heavy alcohol consumption
May slow healing and increase dry mouth.
These factors do not automatically rule out treatment but influence planning.
Bite and jaw structure
Dentists examine the way the teeth meet and where chewing forces concentrate.
An implant in a high-load area may require:
- a wider-diameter implant
- a reinforced crown
- a longer healing period
- bite adjustment
- a protective night guard
Proper occlusal evaluation reduces mechanical stress and long-term complications.
When implants are delayed
Some patients are told elsewhere that they “are not candidates,” but their situation usually requires temporary stabilisation, not permanent exclusion.
Common reasons for delaying implant placement:
- active gum infection
- lack of bone requiring grafting
- uncontrolled diabetes
- heavy smoking without intention to reduce
- cysts or impacted roots needing removal
- residual infection after extractions
- significant sinus involvement
Once stabilised, most patients proceed successfully.
Who makes an ideal candidate
At Maple Dental Health, ideal implant candidates generally have:
- healthy gums with minimal bleeding
- adequate bone height and width
- stable neighbouring teeth
- controlled medical conditions
- consistent oral hygiene
- preference for long-term fixed solutions over removable dentures
Patients who recently lost a tooth often make excellent candidates because bone volume is still strong.
Maple Dental Health’s evaluation process
1. Consultation and medical review
A comprehensive review of dental history, medical conditions, and medications.
2. 3D imaging
A CBCT scan evaluates:
- bone thickness
- location of nerves
- sinus boundaries
- ridge shape and angulation
This imaging ensures accuracy during planning and surgery.
3. Gum and bite assessment
The team examines periodontal stability and the space available for the future crown.
4. Treatment planning
Plans are tailored to each patient and may involve:
- immediate implant after extraction
- staged grafting and later placement
- multiple implants
- full-arch treatment
- implant-supported dentures
Timelines and healing expectations are clearly explained.
5. Maintenance guidance
Long-term success depends on good home care and regular professional cleanings.
As Dr. Mirette Mounir emphasises, “Maintenance is ongoing. An implant must be cared for the same way — or better — than a natural tooth.”
FAQ
What are the criteria for dental implants?
Healthy gums, adequate bone support, controlled medical conditions, and a stable bite.
Who is a poor candidate?
Patients with active gum disease, untreated infections, uncontrolled diabetes, heavy smoking without willingness to reduce, or certain high-dose bone medications.
Who cannot receive an implant?
Permanent contraindications are rare. Severe active jaw infection, intensive bone-affecting cancer therapies, or significant uncontrolled illness may prevent surgery.
Who is the best candidate?
Adults with stable oral health, strong bone, and consistent oral-care habits.
References
Canadian Dental Association — Dental Implants Overview
https://www.cda-adc.ca/en/oral_health/procedures/implants/
Ontario Dental Association — Information on Dental Procedures
https://www.oda.ca
National Institutes of Health (PubMed) — Dental implant survival studies
https://pubmed.ncbi.nlm.nih.gov




















